How does diabetes affect the eye?


Diabetic eye disease is a group of eye problems that can affect people with diabetes. These conditions include diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma. Over time, diabetes can cause damage to your eyes that can lead to poor vision or even blindness.
What are the risk factors making one more prone to diabetic retinopathy?
Poor blood sugar control, high blood pressure, cigarette smoking, obesity and increased lipid levels in the blood, increase the risk of blindness for people with diabetes. It is more likely to occur beyond 5 years of the disease.

How do I know if I have diabetic retinopathy?
As the condition progresses, diabetic retinopathy symptoms may include:
- Spots or dark strings floating in your vision (floaters)

- Blurred vision.
- Fluctuating vision.
- Impaired color vision.
- Dark or empty areas in your vision.

- Vision loss.
What is Diabetic Macular Edema (DME)?


Diabetic Macular Edema (DME) is an accumulation of fluid in the macula part of the retina that controls our most detailed vision abilities—due to leaking blood vessels. In order to develop DME, you must first have diabetic retinopathy.
Is DME serious?
If untreated, chronic macular edema can lead to irreversible damage of the macula and permanent vision loss.
How is Diabetic Macular Edema (DME) treated?


Research has shown that an intravitreal injection often results in better vision than laser treatment alone for patients with diabetic macular edema. The key to these treatments is their ability to block vascular endothelial growth factor (VEGF), a chemical signal that stimulates leakage and abnormal blood vessel growth. The approved treatments are Lucentis (ranibizumab) and Eylea (aflibercept).

Repeated doses of anti-VEGF medications may be needed to prevent blood vessels from leaking fluid and causing vision loss. Some eyes with diabetic macular edema respond better to intravitreal steroid injections than anti-VEGF injections.
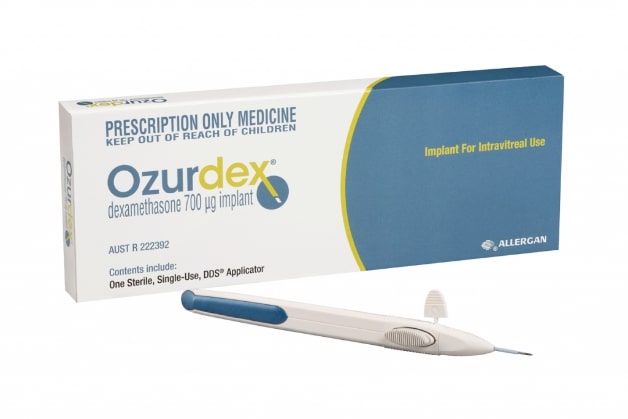
Slow release steroid implants (Ozurdex) has also been shown to be effective. If the swelling does not resolve with injections, laser therapy may be added to improve the response.
How are intravitreal injections performed?
An intravitreal injection is a shot of medicine into the eye. The inside of the eye is filled with a jelly-like fluid (vitreous). During this procedure, your health care provider injects medicine into the vitreous, near the retina at the back of the eye. The medicine can treat certain eye problems and help protect your vision. This method is most often used to get a higher level of medicine to the retina.
How many injections can I expect to need?
Most people who get anti-VEGF injections will need injections once a month for at least the first 3 months. Over time, you may need injections less often. On average, the first year is the most intensive period with most patients needing about 8 injections over 12 months.
I’m terrified of pain – how painful are injections into the eye?
Adequate numbing drops will be applied to ensure that the procedure is fast and painless. Typically, patients feel pressure, with little or no pain during the injection. You may also feel a slight burning sensation that is related to the antiseptic used to clean the surface of the eye. The entire process takes about 10 to 15 minutes.
What are the possible complications of the procedure?
Severe complications are very rare with intravitreal injections. The major risks are:
- Infection in the eye or endophthalmitis
- Inflammation in the eye
- Bleeding into the vitreous gel (vitreous hemorrhage)
- Retinal detachment
- Sometimes there may be a small bleed or subconjunctival hemorrhage on the surface of the eye where the needle enters; this usually heals within a week.
- Temporary rise in eye pressure that usually returns to baseline in a few minutes. If excessively high, your doctor may perform a minor procedure called paracentesis to draw a small amount of fluid from the eye to relieve the pressure quickly.
What steps can I take to avoid infection after the procedure?
It is important to avoid rubbing the eye as the most common source of infection is from skin bacteria. You should also try to keep the eye as dry as possible especially when taking a shower. You should not swim for at least a week after injection. Besides these, you may return to normal activities after 1-2 days, including driving, reading, watching television and light exercise.
What should I look out for after the injection?
You might notice a few floaters or small bubbles appearing in the corner of your vision after the injection. These are normal and will disappear within 2-3 days.
However, you should contact your ophthalmologist if you experience signs and symptoms of complications, such as:
- Eye pain
- Decreased vision
- Seeing many floaters after the first day
- Increased sensitivity to light
What is Proliferative Diabetic Retinopathy (PDR)?


Proliferative retinopathy is a developed form of retinopathy whereby new but weak blood vessels begin to form on the retina to help restore blood supply.
How is Proliferative Diabetic Retinopathy (PDR) treated?


When proliferative diabetic retinopathy develops, this is treated with a laser treatment called pan retinal photocoagulation (PRP) and possibly anti-VEGF injections.
Vitrectomy surgery (removal of the vitreous) may be used in eyes with vitreous hemorrhage or severe scar tissue on the retina (epiretinal membrane or traction retinal detachment).
What can I do to prevent diabetic complications of the eye from happening?


If you have diabetes, keep your health on track:
- Take your medicines as prescribed by your doctor
- Reach and maintain a healthy weight
- Add physical activity to your day
- Control your ABCs—A1C, blood pressure, and cholesterol
- Kick the smoking habit
Regular dilated eye exams reduce the risk of developing more severe complications from the disease.
It is extremely important for diabetic patients to maintain the eye examination schedule put in place by the ophthalmologist. How often an examination is needed depends on the severity of your disease. Through early detection, the ophthalmologist can begin a treatment regimen.