What is Central Serous Chorioretinopathy (CSC)?


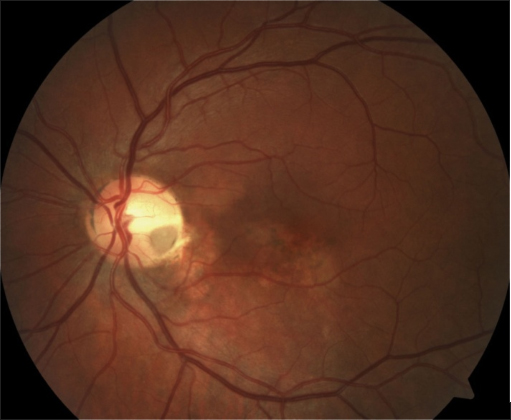
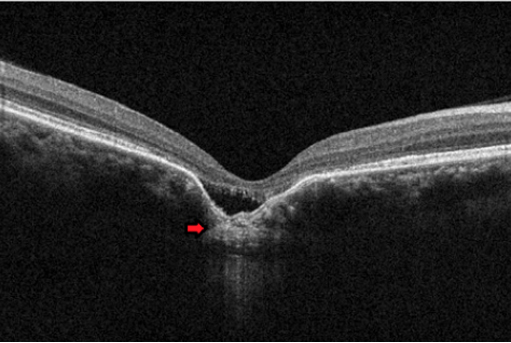
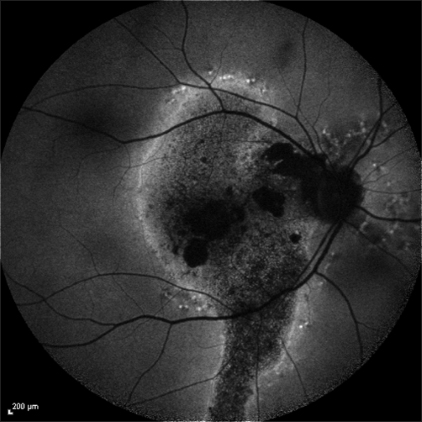
Central serous chorioretinopathy, commonly referred to as CSC, is a condition in which fluid accumulates under the retina, causing a serous (fluid-filled) detachment and vision loss.
What are the symptoms of CSC?


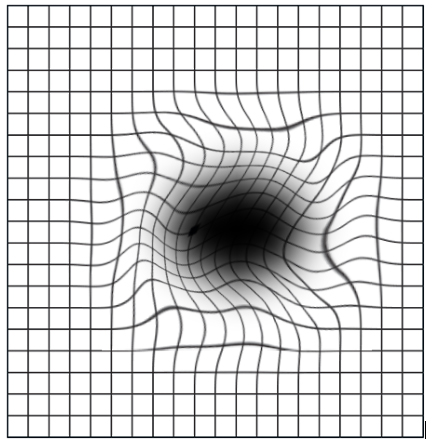
Blurry central vision, which often occurs in one eye, is the most common symptom that patients experience; however, careful examination often reveals some involvement in the other eye as well. Other symptoms include distortion of grid lines and micropsia, a phenomenon where an object appears smaller or further away when viewed with the affected eye compared to the normal eye.
Depending on the location and amount of subretinal fluid, CSC can show no symptoms, especially if the affected areas fall outside of the macula
What causes CSC?


The exact cause is still unknown. It is thought that any exposure to a corticosteroid drug can bring about or worsen CSC. Corticosteroids are found in allergy nose sprays and anti-inflammatory skin creams available over the counter, and are often prescribed to treat a variety of medical conditions.
An association has also been made between CSC and patients with emotional stress and/or “type A” personalities. It is possible that the body over-produces natural corticosteroids in times of stress that may trigger CSC in an individual prone to this condition.
About half of patients diagnosed with CSC have at least one relative with findings of the disease on retinal examination. This indicates that there may be a genetic tendency; however, no specific inheritance pattern has been identified.
Patients with high blood pressure or heart disease, and those with a current or recent pregnancy have been shown to have a higher risk of developing CSC.
Beyond corticosteroids, there is evidence that other drugs including stimulants, decongestants, erectile dysfunction medications, and some anti-cancer agents (e.g. MEK or mitogen activated protein kinase) inhibitors) may trigger CSC. Be sure to tell your doctor about any medication you are taking.
There are rare congenital anomalies such as focal choroidal excavation and optic disc pit that may predispose to CSC.
Do all cases need treatment?


There are 2 different types of CSC: acute and chronic. In the acute form, the disease is usually self-limiting, and visual recovery usually occurs within a few weeks to months without treatment. If it persists beyond 3 months, then treatment should be considered. For occupations that require good binocular vision, treatment may be undertaken even earlier than 3 months.
Patients who are taking corticosteroids of any kind should discontinue their use if possible, but only after checking with their prescribing physician to ensure it is safe to stop. Suddenly discontinuing high-dose steroid medications can cause medical problems.
However, in the chronic form of CSC, almost all patients invariably lose vision because of scarring and thinning of retinal tissue. Hence all case of chronic CSC should be treated.
What are the treatment options?


Several therapies have been used to treat chronic CSC, including thermal laser treatments, oral medications, and eye injections.
The oral medication prescribed is Eplerenone. Typically, patients have to be on this treatment for at least one month. There are side effects which may limit its use, for example raised serum potassium levels, fatigue and muscle cramps. A recent randomised trial showed no benefit of this treatment over placebo.
A “cold laser,” called photodynamic therapy, is also effective and often used to focally treat the source of fluid leakage under the retina in chronic CSC.
With photodynamic therapy, a drug called verteporfin is injected into the arm, where it travels to the eye. The verteporfin is activated by shining a special cold laser on the source of leakage in chronic CSC. It may also prevent future recurrences in some eyes.