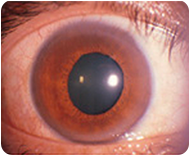
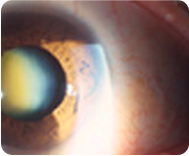
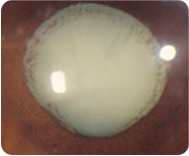
Cataracts are opacities in the normally clear human lens which blur vision; they generally occur with advancing age or as a result of some insult e.g. injury, drugs, inflammation. Everybody will get a cataract if they live long enough. Here is what cataracts look like:
The surgery is quick and painless and vision returns rapidly.
At Eye and Retina Surgeons, it is no longer good enough to just remove a cataract and hope for a good visual result using glasses. It is part of our practice philosophy to try and give our patients good vision after cataract surgery without glasses or other visual aids.
Our aim for our patients is: Good Unaided Vision!
To achieve this requires attention to many details prior to surgery.
- Consultation and Assessment
- Biometry (Accurate measurements of the axial length of your eye and the corneal curvature)
- Selection of Intraocular Lens Implant (IOL)
- Surgical planning
Consultation and Assessment


During your consultation, your pupils will be dilated so that the density and hardness of your cataract can be assessed.
This has a bearing on the selection of the machine used to remove your cataract. The harder and more mature cataracts will usually require more sophisticated equipment. Your eye will be assessed for other conditions which may have a bearing on the outcome of your surgery. Eg glaucoma, diabetic retinopathy, age-related macular degeneration. Your refractive state will be assessed: myopia, hyperopia, astigmatism and presbyopia.
Your doctor will then advise you as to whether you will benefit from cataract surgery and discuss the options with you.
Biometry


Once the decision has been made that you will benefit from cataract surgery, measurements need to be taken of your eye so that we can choose the most appropriate lens implant to replace your cataractous lens. This is called biometry. Remember that if we take your cataract out, we are actually taking your lens out and we need to replace it with an artificial one to allow you to see again.
We have equipments (IOL Master 700, Sonomed, Pentacam) that will measure the length of your eyeball and the curvature of your cornea. With these measurements, we will then have all the information we need to calculate and make an informed decision on the most suitable lens for you and your lifestyle.
Selection of Intraocular Lens Implant (IOL)


Currently there are three major classes of lens implants:

These IOLs are simple and yet give good visual results. Because they are monofocal in nature, in general they give good quality of vision as few compromises are made in their design. Optically speaking, all lens systems should be aspheric in design. Many companies manufacture excellent monofocal implants and one of the latest monofocal designs that has been impressive is the Eyhance implant from Johnson & Johnson. The Alcon Natural Aspheric Lens Implant is another excellent lens.
Toric IOLs
Toric lens implants can correct pre-existing corneal astigmatism. Astigmatism is present in many of us and results in blurring of vision which usually requires glasses to correct. (Astigmatism is a condition of the eye in which the transparent cornea is shaped like a part of an egg rather than a sphere).
Previously, nothing could be done about astigmatism after cataract surgery apart from glasses or LASIK. The Toric implants now available have shown good results in giving good quality vision after cataract surgery without using glasses. It requires accurate implant placement.

Toric Lens Implant: Note the line of 4 dots on each side of the lens which aligns with astigmatic axis.
Multifocal IOLs
One of the main problems after traditional cataract surgery with a monofocal lens implant is that the eye is normally 'set' for good distance vision. Reading requires reading glasses.
This condition is called surgical presbyopia or 'lao hwa yen'. Physiological presbyopia occurs after the age of 40 in all patients.
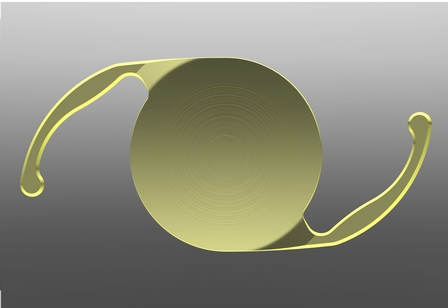
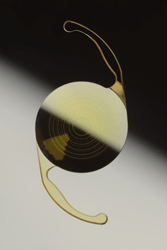
A multifocal lens implant with diffractive rings.
Multifocal lens implants like the Tecnis or Restor bifocal implant allow a post-cataract surgery patient to see well for far as well as near without the need for glasses at all. Dr Yeoh was an early user of the first generation Restor multifocal lens implant when it was introduced to Singapore in 2004. Indeed, Dr Yeoh is a trainer for many surgeons in the Asia-Pacific who learnt to use this lens.
Dr Yeoh found that more than 90% of his patients after the Restor lens was implanted did not need glasses at all.
The Restor bifocal IOL has now been superceded by the trifocal Panoptix IOL which gives a full range of vision.
The Panoptix multifocal lens implant: note the concentric rings in the lens which confer the power of multifocality.
The latest generation presbyopia correcting IOL is known as the Synergy lens implant and this has both trifocal and extended depth of focus (EDOF) capabilities giving patients an impressive range of vision from infinity all the way down to 33cm.

Trifocal and EDOF Synergy IOL
Patients who wish to have these more sophisticated lens implants should have healthy eyes with no other problems apart from cataract. They will then gain maximal benefit from these implants.
Some patients are unable to have a multifocal or accommodative lens implant inserted because they have high astigmatism or extreme myopia/hyperopia. For these patients, the concept of monovision may well be effective in giving a range of far and near vision. In the monovision option, the first eye that is operated is targeted for a close to zero degree outcome which gives good distance vision, but relatively poor near vision (that’s just physics at work!) The second eye that has the cataract surgery is then targeted for about -1.5D or 150 degrees myopia. With this level of myopia, a patient can have what I term ‘social reading vision’ ie computer usage, filling in forms, reading menus and importantly putting on and taking off make up! The two eyes blend the distant and near vision to give an effective range of vision. As the disparity between the two eyes is only about 1.5D or 150 degrees, the eyes and brain are quite comfortable with this arrangement. (A difference of up to 4D or 400 degrees is tolerable)
Note that some implants shown above have a light yellow tint which mimics the colour of the natural human lens and offers retinal protection from potentially harmful blue light wavelengths. It is incorporated some lens designs for this reason.
The use of standard monofocal aspheric lens implants to replace a cataract and correct myopia or hyperopia is commonly practiced. In the past few years, Toric implants to correct pre-existing corneal astigmatism and multifocal lens implants to correct presbyopia (reading difficulty) have become established in an effort to reduce spectacle dependency after cataract surgery.
Planning for surgery


Modern cataract surgery uses ultrasound to break up a cataract into small pieces so that it can be sucked out through a tiny 2.2 – 2.6mm incision. This operation is known as phacoemulsification (phaco) of cataract with insertion of a foldable lens implant.
Traditional phaco uses longitudinal movements of a metal tipped instrument (the phacotip) to break up the nucleus. Whilst this is effective, there are a few drawbacks; the back and forth movement of the phacotip results in wasted energy on the backward stroke and unwanted heat generation potentially causing damage to the eye. This movement also sometimes caused parts of the nucleus to fly away from the phacotip during the forward stroke resulting in inefficiency and potential damage to the eye.
Another way of removing cataracts by using a design in which the phacotip moved from side to side was invented by American eyecare company Alcon. This is called Ozil or torsional Phaco. This overcame both the above problems effectively. Torsional phaco is now available in the current iteration of the phaco machine; the Centurion which features more stable fluidic platforms and more efficient phacotips.

The Centurion phaco machine
This machine allows efficient removal of cataracts quickly and reliably, especially for complicated and difficult cataracts.
In general, your operation will take about 30 minutes is almost always done under local anaesthesia; regional (injection or topical (eye- drop) as day case surgery. An anaesthetist will stand by to monitor your general condition and deal with any medical situations that may arise.
The operation is painless and you can expect have clearer vision by the next morning.
Femtolaser assisted cataract surgery (FLACS)
An exciting paradigm shift in cataract surgery technique has become increasingly popular in the last year. True laser cataract surgery is here now. Where ‘standard’ cataract surgery involves making incisions with blades and manually opening up the cataract capsule (capsulorhexis) with needles and forceps and breaking up the hard core (nucleus) of the cataract by ultrasound energy and a metal’ chopper’ , FLACS is now bladeless cataract surgery and the use of the laser to open up the cataract capsule and break up the nucleus is more accurate and uses less ultrasound energy. This results in more accurate outcomes and safety.
The accuracy of the refractive outcome; something which is increasingly important with the use of lens implants (AT IOLs) like multifocal and multifocal toric lens implants. Ideally, we should try and achieve a close to zero degree outcome and there is increasing evidence that FLACS gives us these more accurate refractive outcomes.
Surgeons at ERS have access to the most commonly used Femtolaser , the Lensx system supplied by Alcon (Fig 1). This system is able to make incisions, open up a perfectly round opening in the cataract and then divide up the nucleus efficiently and safely.

Figure 1
The Lenx Femtolaser System
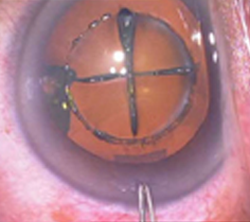
Figure 2
Perfectly circular opening in cataract capsule (Capsulorhexis) and a cross dividing nucleus into 4 quarters. A perfectly constructed incision is also seen where the pair of forceps is about to enter the eye.
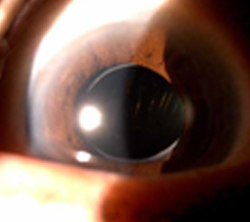
Figure 3
Perfectly round opening in cataract capsule with lens implant perfectly centered
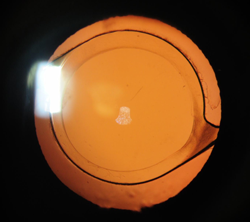
Figure 4
Perfectly positioned lens implant within the femtosecond laser created central capsular opening
What can you expect with FLACS?
FLACS (bladeless cataract surgery) starts off with the femtolaser step in which the incisions, capsulorhexis and nuclear division are done under topical (eye drop) anaesthesia. The eye then looks like Fig 2 above. You will then be moved over to another operating room where the incisions are opened up, the cataract removed using less ultrasound energy and an appropriate lens implanted. It is a painless and quick procedure.
Post-operatively it is to be expected that the eye is a little redder than normal due to the suction applied during the laser step. This redness will fade in 1-2 weeks. This is what a well performed FLACS eye looks like a month after surgery Fig 3 and Fig 4.
Whilst this technology is undoubtedly attractive, not every patient is suitable for FLACS. Your doctor will discuss the pros and cons and help you decide whether to have a standard procedure or a FLACS (bladeless cataract surgery) procedure. Please feel free to ask for more information.
Drs Ong and Yeoh were early adopters of FLACS techniques in Singapore. Dr Yeoh is a trainer for Alcon in training surgeons beginning FLACS and conducts many round table discussions on adopting FLACS. He has also used all the FLACS platforms from different manufacturers that are available in Singapore today: the Lensx from Alcon, the Catalys from AMO, the Victus from Bausch and Lomb and the Z8 from Ziemer.
Post-operative recovery
The eye may feel slightly uncomfortable a few hours after surgery when the anaesthetic wears off. In general, there should not be much pain. You will be given an eye shield to wear at night so that you do not rub your eyes accidentally in your sleep.
Eye drops will be given to prevent eye infection and inflammation.
After 3-4 weeks, your eye should be stable and a refraction will be done to see if you need glasses. If so, glasses can be made at this stage.
Summary
In the past, cataract surgery tended to be done only in elderly patients whose cataracts were ‘ripe’ and the objective was to give the cataract patient back his eye sight with the use of glasses.
This mindset has now changed because with the current techniques of removing cataracts and the current range of lens implants, cataract surgery has now become lifestyle surgery where apart from merely removing an opaque lens and replacing it with a standard lens, we can now give good vision to everyone with cataracts. Indeed, many patients with early cataracts often choose to undergo early cataract surgery so they do not need to wear glasses!




